LCSNW clients must stay alert as COVID-19 emergency benefits and rules lapse
 A couple of important changes are coming to clients and staff of Lutheran Community Services Northwest, due to the end of the national Public Health Emergency (PHE) this spring. LCSNW has lifted its masking requirements in our health care settings effective April 3, the same date set by Washington and Oregon health authorities to end the COVID-19 order in place since 2020.
A couple of important changes are coming to clients and staff of Lutheran Community Services Northwest, due to the end of the national Public Health Emergency (PHE) this spring. LCSNW has lifted its masking requirements in our health care settings effective April 3, the same date set by Washington and Oregon health authorities to end the COVID-19 order in place since 2020.
The other change will affect our Medicaid clients in Washington and Oregon. Over the past three years, many clients have received extended federal coverage, services and support due to the PHE. Some temporary programs and eligibilities will end as the PHE phases out over the next several months, which will affect millions of Americans. Benefits that will be impacted include health insurance and support for people with disabilities and older adults, and food benefits.
 There’s no need to panic. Officials will start reviewing Medicaid eligibility in April and for the remainder of 2023. Clients will receive information letters that include next steps, if any, necessary to retain benefits administered by the states of Washington and Oregon. Both states say their goal is to keep as many people as possible connected to benefits and covered by a health plan.
There’s no need to panic. Officials will start reviewing Medicaid eligibility in April and for the remainder of 2023. Clients will receive information letters that include next steps, if any, necessary to retain benefits administered by the states of Washington and Oregon. Both states say their goal is to keep as many people as possible connected to benefits and covered by a health plan.
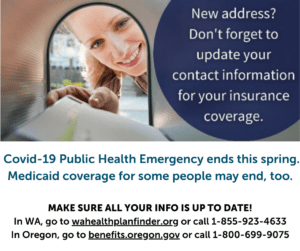
At LCSNW, we want to make sure our Medicaid clients continue to get the help they need, and that Washington and Oregon state officials can reach them. This means clients must provide their current address and that they open and respond to letters sent by the state.
Here are the recommendations we are giving to clients:
- Has your mailing address, phone number or email address changed? If yes, update your information online at wahealthplanfinder.org or benefits.oregon.org
- Pay close attention to your mail. The letter from the state will let you know what you need to do to see if you still qualify for Medicaid benefits.
- Complete your renewal form (if you get one) – Fill out the form and return it to the state right away. Even if you no longer qualify for OHP, Washington Apple Health or other benefits, it’s important to respond to the state’s letter so they can help you find other coverage.
- If you need help, you may assign an authorized representative who can be a family member or friend you choose to help you. Language interpretation services are also available.
- For assistance by phone: In Washington call 1-855-923-4633 (or visit your local Community Service Office) and in Oregon call 1-800-699-9075.
We are providing print handouts at our LCSNW offices, taking phone calls from clients, and doing all we can to ensure they stay alert and stay eligible for benefits.

0 Comments